Story: https://www.snmmi.org/NewsPublications/NewsDetail.aspx?ItemNumber=43664
Reston, VA—A new nuclear medicine therapy can cure human non-Hodgkin lymphoma in an animal model, according to research published in the April issue of The Journal of Nuclear Medicine. A single dose of the radioimmunotherapy, [177Lu]Lu-ofatumumab, was found to quickly eliminate tumor cells and extend the life of mice injected with cancerous cells for more than 221 days (the trial endpoint), compared to fewer than 60 days for other treatments and just 19 days in untreated control mice.
Non-Hodgkin lymphoma is a common blood malignancy. The American Cancer Society estimates that more than 80,500 new cases and 20,100 deaths will occur in the United States in 2023. The standard of care for many non-Hodgkin lymphoma patients involves chemotherapy and immunotherapy targeting the CD20 protein, which is highly expressed on most non-Hodgkin lymphoma cells.
“Although this chemotherapy with immunotherapy combination is usually initially effective, many patients don’t respond or relapse, so we need improved therapies,” said Richard L. Wahl, MD, the Elizabeth E. Mallinckrodt Professor and director of Mallinckrodt Institute of Radiology at Washington University School of Medicine in St. Louis, Missouri.
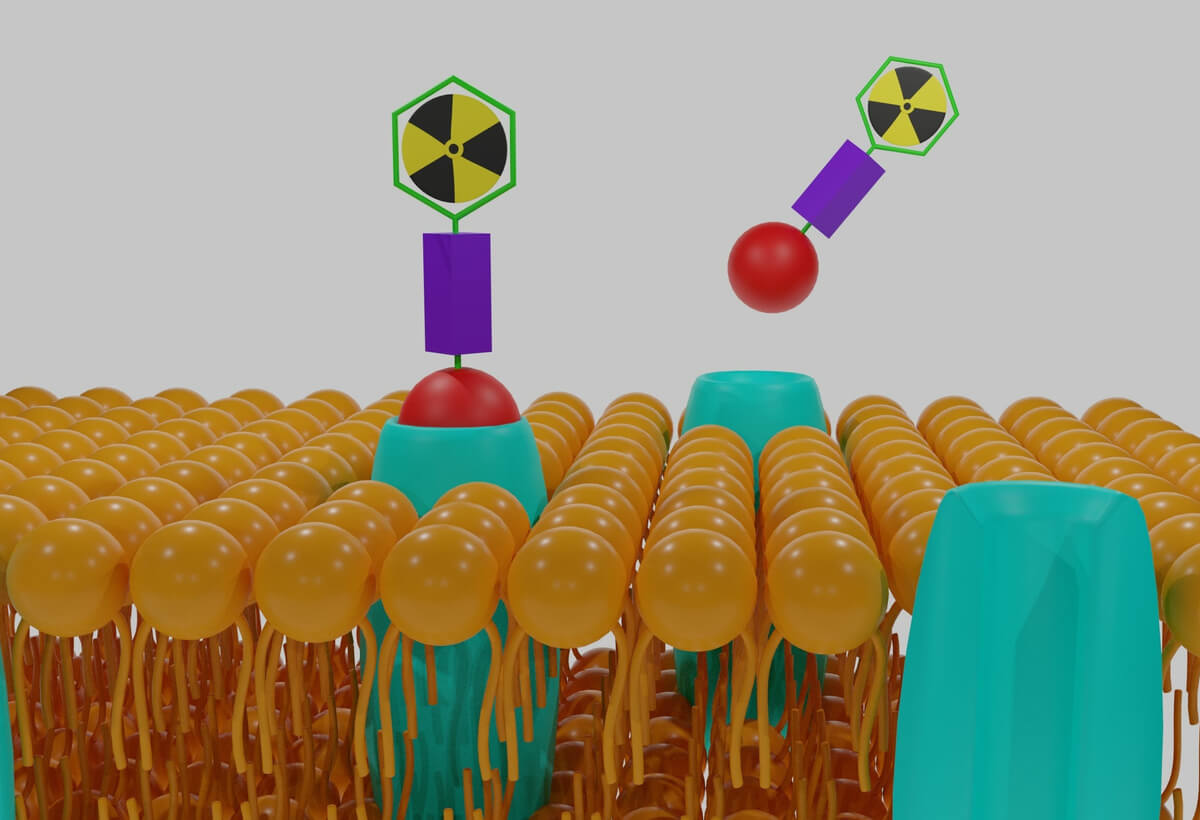
In the study researchers labeled ofatumumab, a recently developed anti-CD20 fully human antibody, with 177Lu, a widely used therapeutic radioisotope that can kill cancer cells. They then determined the in vitro characteristics of [177Lu]Lu-ofatumumab, estimated human dosimetry, and evaluated its therapeutic effectiveness for non-Hodgkin lymphoma in a mouse model.
The most significant finding of the study came from the preclinical therapy trial. Mice injected with human B cell lymphoma were either untreated, treated with unlabeled ofatumumab, treated with 8.51 MBq of [177Lu]Lu-IgG, or treated with 0.74 MBq or 8.51 MBq of [177Lu]Lu-ofatumumab. The best results occurred with 8.51 MBq of [177Lu]Lu-ofatumumab, for which the median survival was more than 221 days, essentially curing the mice. The median survival of untreated mice and those treated with unlabeled ofatumumab, [177Lu]Lu-IgG, and 0.74 MBq of [177Lu]Lu-ofatumumab was 19, 46, 25 and 59 days, respectively.
“What’s more, in mice treated with 8.51 MBq of [177Lu]Lu-ofatumumab, detectable tumors were eliminated completely within two days. Mice treated with the other therapies or left untreated, on the other hand, continued to show tumor cells present,” Wahl explained.
Researchers were able to produce [177Lu]Lu-ofatumumab with high yield and high purity. It showed favorable in vitro characteristics and dosimetry estimates that support the feasibility of human translation.
“The excellent therapeutic results in this animal model of human B cell lymphoma suggest that this curative treatment should be tested in humans with non-Hodgkin lymphoma,” noted Wahl. “If testing is successful in humans, this would represent an excellent new treatment option for patients with this disease.”

| Figure 4. Bioluminescence images of untreated and treated mice with human B cell lymphoma. Optimal results occurred with 8.51 MBq of [177Lu]Lu-ofatumumab (bottom row). Ofa = ofatumumab. |
The authors of “Cure of disseminated human lymphoma with [177Lu]Lu-ofatumumab in a preclinical model” include Kyuhwan Shim, Mark S. Longtine, Diane S. Abou, Mark J. Hoegger, and Richard S. Laforest, Mallinckrodt Institute of Radiology, Washington University, St. Louis, Missouri; Daniel L. J. Thorek, Mallinckrodt Institute of Radiology, Washington University, St. Louis, Missouri, and Department of Biomedical Engineering, Washington University, St. Louis, Missouri; and Richard L. Wahl, Mallinckrodt Institute of Radiology, Washington University, St. Louis, Missouri, and Department of Radiation Oncology, Washington University, St. Louis, Missouri.
Visit the JNM website for the latest research, and follow our new Twitter and Facebook pages @JournalofNucMed or follow us on LinkedIn.
###
Please visit the SNMMI Media Center for more information about molecular imaging and precision imaging. To schedule an interview with the researchers, please contact Rebecca Maxey at (703) 652-6772 or rmaxey@snmmi.org.
About JNM and the Society of Nuclear Medicine and Molecular Imaging
The Journal of Nuclear Medicine (JNM) is the world’s leading nuclear medicine, molecular imaging and theranostics journal, accessed 15 million times each year by practitioners around the globe, providing them with the information they need to advance this rapidly expanding field. Current and past issues of The Journal of Nuclear Medicine can be found online at http://jnm.snmjournals.org.
JNM is published by the Society of Nuclear Medicine and Molecular Imaging (SNMMI), an international scientific and medical organization dedicated to advancing nuclear medicine and molecular imaging—precision medicine that allows diagnosis and treatment to be tailored to individual patients in order to achieve the best possible outcomes. For more information, visit www.snmmi.org.
Summary:
Scientists have developed a new nuclear medicine treatment that can cure non-Hodgkin lymphoma, a common blood cancer, in mice. The therapy, called [177Lu]Lu-ofatumumab, uses a radioimmunotherapy that quickly eliminates cancerous tumor cells and extends the life of mice that were injected with the disease. The trial found that a single dose of the treatment cured the mice for over 221 days, compared to 60 days with other treatments and 19 days in untreated mice. The study also showed that the therapy eliminated detectable tumors within two days, while untreated mice continued to show tumor cells present. Non-Hodgkin lymphoma is estimated to cause over 80,500 new cases and 20,100 deaths in the United States in 2023. The current standard treatment for many non-Hodgkin lymphoma patients involves chemotherapy and immunotherapy targeting the CD20 protein. However, many patients don’t respond to these treatments or relapse, highlighting the need for improved therapies. The researchers are hopeful that the treatment will be tested in humans, representing a new treatment option for patients with non-Hodgkin lymphoma